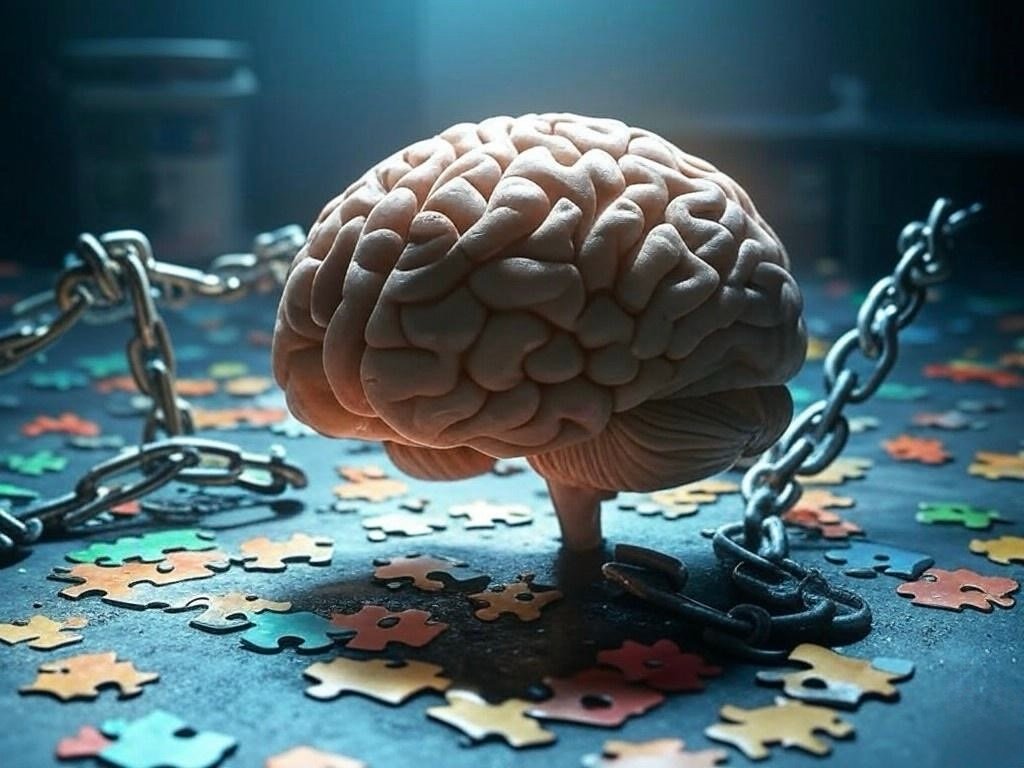
The “chemical imbalance” theory, which posits that mental illnesses like depression are caused by imbalances in brain chemicals such as serotonin, has been a dominant narrative in psychiatry for decades. Despite mounting evidence challenging its validity, this theory persists in public consciousness and clinical practice. Understanding the reasons behind its endurance requires an exploration of historical, commercial, and psychological factors.
Historical Context and the Rise of the Chemical Imbalance Theory
In the mid-20th century, psychiatry sought to establish itself as a rigorous medical discipline by identifying biological bases for mental disorders. The introduction of selective serotonin reuptake inhibitors (SSRIs) in the late 20th century bolstered the chemical imbalance narrative, as these medications were believed to correct presumed serotonin deficiencies associated with depression. This perspective was appealing due to its simplicity and the promise of straightforward pharmacological treatments.
Commercial Influence and Public Perception
Pharmaceutical companies played a significant role in promoting the chemical imbalance theory. Marketing campaigns for SSRIs and other psychotropic medications often emphasized their ability to rectify chemical imbalances, embedding this concept into public consciousness. A study examining media reports found that the idea of neurotransmitter imbalances causing depression was vigorously promoted by pharmaceutical companies and the psychiatric profession at large.
Psychological Appeal of the Theory
For many individuals, the chemical imbalance explanation offers a tangible and non-stigmatizing understanding of their mental health struggles. Attributing symptoms to a biochemical cause can alleviate feelings of personal failure or moral weakness, making the theory psychologically comforting and socially acceptable.
Challenges to the Chemical Imbalance Theory
Recent scholarly reviews have critically evaluated the evidence supporting the serotonin-depression link. For instance, a comprehensive review concluded that there is no consistent evidence of an association between serotonin and depression, and no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations.
Additionally, the efficacy of antidepressants has been called into question. Some meta-analyses suggest that the difference between antidepressants and placebos is minimal, especially in cases of mild to moderate depression. This challenges the notion that these medications work by correcting a chemical imbalance.
The Persistence of the Theory
Despite these challenges, the chemical imbalance theory remains prevalent. Several factors contribute to its persistence:
• Entrenched Beliefs: Both clinicians and patients have been exposed to this narrative for decades, making it a deeply ingrained belief that is resistant to change.
• Pharmaceutical Interests: The continued marketing of medications that are purported to correct chemical imbalances reinforces the theory.
• Lack of Public Awareness: Scientific debates and paradigm shifts within psychiatry may not be effectively communicated to the public, allowing outdated theories to persist.
Moving Forward
The endurance of the chemical imbalance theory underscores the need for a more nuanced understanding of mental health. Mental illnesses are complex, with biological, psychological, and social dimensions. Embracing a biopsychosocial model can lead to more comprehensive and individualized treatment approaches.
In conclusion, while the chemical imbalance theory has been instrumental in shaping modern psychiatry and reducing stigma, it oversimplifies the multifaceted nature of mental illness. Ongoing research and open dialogue are essential in advancing our understanding and treatment of mental health conditions.
Below are the sources used in my article, for additional information contact me at rami.nasser@bullcitycitizen.com
1. Moncrieff, J., Cooper, R. E., Stockmann, T., Amendola, S., Hengartner, M. P., & Horowitz, M. A. (2022). The serotonin theory of depression: A systematic umbrella review of the evidence. Molecular Psychiatry. https://discovery.ucl.ac.uk/id/eprint/10147405/
2. Lacasse, J. R., & Leo, J. (2005). Serotonin and depression: A disconnect between the advertisements and the scientific literature. PLoS Medicine, 2(12), e392. https://doi.org/10.1371/journal.pmed.0020392
3. Kirsch, I., Deacon, B. J., Huedo-Medina, T. B., Scoboria, A., Moore, T. J., & Johnson, B. T. (2008). Initial severity and antidepressant benefits: A meta-analysis of data submitted to the Food and Drug Administration. PLoS Medicine, 5(2), e45. https://doi.org/10.1371/journal.pmed.0050045
4. Whitaker, R. (2010). Anatomy of an epidemic: Magic bullets, psychiatric drugs, and the astonishing rise of mental illness in America. Crown Publishing Group.
5. Read, J., Cartwright, C., & Gibson, K. (2014). How many of 329 antidepressant trials published by 2013 had positive results? A critique of Moncrieff and Kirsch (2005). Journal of Social Work Practice, 28(4), 475-479. https://doi.org/10.1080/02650533.2014.925861
6. France, C. M., Lysaker, P. H., & Robinson, R. P. (2007). The “chemical imbalance” explanation for depression: Origins, lay endorsement, and clinical implications. Professional Psychology: Research and Practice, 38(4), 411–420. https://doi.org/10.1037/0735-7028.38.4.411
7. Healy, D. (2015). Serotonin and depression. BMJ, 350, h1771. https://doi.org/10.1136/bmj.h1771
8. Harrow, M., & Jobe, T. H. (2013). Does long-term treatment of major mental illness with antipsychotic medications facilitate recovery? Psychological Medicine, 43(12), 2545–2555. https://doi.org/10.1017/S0033291713001340